Abstract
Background:Little is known about the long-term effects of high-deductible insurance on care for chronic medical conditions.
Objective:To determine whether a transition from low-deductible to high-deductible insurance is associated with delayed medical care for macrovascular complications of diabetes.
Design:Observational longitudinal comparison of matched groups.
Setting:A large national health insurer during 2003 to 2012.
Participants:The intervention group comprised 33 957 persons with diabetes who were continuously enrolled in low-deductible (≤$500) insurance plans during a baseline year followed by up to 4 years in high-deductible (≥$1000) plans. The control group included 294 942 persons with diabetes who were enrolled in low-deductible plans contemporaneously with matched intervention group members. Intervention:Employer-mandated transition to a high-deductible plan.
Measurements:The number of months it took for persons in each study group to seek care for their first major macrovascular symptom, have their first major diagnostic test for macrovascular disease, and have their first major procedure-based treatment was determined. Between-group differences in time to reach a midpoint event rate were then calculated.
Results:No baseline differences were found between groups. During follow-up, the delay for the high-deductible group was 1.5 months (95% CI, 0.8 to 2.3 months) for seeking care for the first major symptom, 1.9 months (CI, 1.4 to 2.3 months) for the first diagnostic test, and 3.1 months (CI, 0.5 to 5.8 months) for the first procedure-based treatment.
Limitation:Health outcomes were not examined.
Conclusion:Among persons with diabetes, mandated enrollment in a high-deductible insurance plan was associated with delays in seeking care for the first major symptoms of macrovascular disease, the first diagnostic test, and the first procedure-based treatment.

This will probably exterminate us before global warming does. Or maybe a supervirus is first.
For every cardiology patient visualise the status of the following stuff:
1. Electrical Rhythm and conduction
Tachyarrhytmias, bradyarrhytmias, heart blocks, pacemakers
2. Coronary arteries
Coronary artery disease, risk factors, Stress-test/angiograms/scan?, PCI or CABG history?
3. Heart muscle function
Cardiomyopathies,
4. Valve function
Regurgitation, stenosis
5. Accesories
pericard, vasculator (aorta), systemic diseases affecting the heart (DM2), elektrolytes, pulmonary function


Case: A 50 year old male with alcohol abuse present in the Emergency department with mild chest pain. He has been nautious and vomiting the past couple of days. Also there is diffuse abdominal tenderness. He gets admitted to control pain and CT-scan next days but detiorates suddenly. He dies. Obduction shows a ruptured oesophagus.
Boerhaave syndrome is rupture of esophagus and rapidly fatal.
History: a dutch grand admiral was retching and tore his oesophagus apart. He died after eating a duck.
Pathofysiolygy: rupture of esophagus due to increase intraluminal pressure usual due to vomiting or retching. Alcohol intake is related. Higher risk if gastro-intestinal disease is present.
Other causes: straining, childbirth, heavy lifting, seizures, fits of coughing or hiccup
Clinical symptoms: chest pain, nautious, vomiting (bloody), dysphagia, dyspnea,
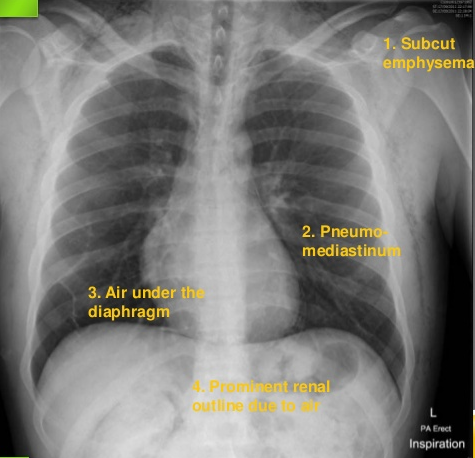
Anderson Triad: Subcutaneous emphysema, rapid respirations, and abdominal rigidity
Macler triad: vomiting, pain, subcutaneous emphysema
Physical examination: Crepitus in the neck, abdominal rigidity, abdominial pain. tachycardia, tachypnoe
Chest X-ray signs:
If still suspected make CT-thorax/abdomen (contrast in esophagus?).
Treatment:
* Surgery as soon as possible
Aggresive resuscitation and broadspectrum antibiotics.
The cause of death is usually polymicrobial septic shock and mediastinitis.